The following essay started as a technical analysis of the disparities in American healthcare between rural and urban communities. It was originally written in an academic style with very dry language and the use of vocabulary words that are not well known outside the field of healthcare administration. However, the essay has been revised into a summary of the healthcare system in rural America, and a persuasive argument in favor of moving towards a socialistic system of healthcare. The purpose of this is to demystify the healthcare system for American workers, to reveal the contradictions laying at the base of the system and explain how they have led to the system’s many failures. Any thorough analysis of the U.S. healthcare system such as this will blatantly reveal the contradictions of capitalism itself, and the many ways that capital has infected American healthcare.
Additionally, this analysis critiques the toothless ‘solutions’ to the problems in healthcare being proposed by ‘healthcare policy experts.’ While these experts are deeply knowledgeable about the existing system, they almost always overlook the blatant contradiction between the profit motivations of healthcare capitalists, and the intended goal of the system, which is to maximize health outcomes for the population. Policy experts generally suggest technocratic changes to the system, which never threaten the billions of dollars in revenue that shareholders make from the system each year. Solutions produced by these policy experts are often funded by enormous healthcare conglomerates such as United Health Group Inc. Therefore, the very companies who constitute the root of the healthcare system’s problems, are those who oversee producing solutions for fixing the same problems they caused. This shows how deeply capital has infected the system and captured the discourse surrounding it.
The Deficiencies in Rural Healthcare & Solutions Being Proposed
One of the primary healthcare concerns that has plagued the rural United States for decades has been lack of access to hospitals and emergency care. Rural America has a general shortage of physicians and healthcare professionals, a lack of sufficient healthcare facilities, and has experienced overall economic stagnation throughout the last 40 years. Four decades of neoliberalism, the political-economic ideology favoring unregulated capitalism and minimal social safety net, has battered the economies and healthcare systems of most every town in the rural U.S. In the last decade alone over 100 rural hospitals were shut down due to lack of revenue, leaving many rural residents without access to a hospital within a reasonable distance. An overall shift in healthcare, towards outpatient care and away from inpatient, has also contributed to the falling number of rural hospitals.
Various solutions have been proposed to tackle the issue of declining rural hospital access. Many policy experts have called for Freestanding Emergency Departments (FSEDs) to provide emergency care for rural areas in desperate need. FSED’s are essentially mobilized emergency care departments, that don’t offer the other services traditionally associated with hospitals. Proponents of FSEDs argue they deliver care faster and are farther reaching than traditional hospitals but are cheaper to maintain as they require less staff. FSEDs have seen some success in practice, however, that success is usually dependent on the economic conditions of the community it’s implemented in, as well as how much Government financing the FSED receives. FSEDs are not a viable solution to the massive problems facing the rural healthcare system. Based on the existing barriers between rural Americans and hospital care, and the consistently decreasing number of hospitals in rural areas, much larger scale changes are needed to improve access to quality hospital care for the rural U.S.
To better understand the problems facing rural America specifically, we can compare relevant health statistics between urban and rural communities. Over the past four decades a large body of literature has been produced detailing the disparities between rural and urban healthcare. A comparative study was done in 2007 analyzing the differences in healthcare quality indicators between urban acute care hospitals and rural critical access hospitals in the U.S. Of the 12 quality indicators measured, 8 showed a statistically significant difference between urban and rural, with 7 of the 8 favoring the urban acute care hospitals (Lutfiyya, 2007). The study concluded that urban communities have access to higher quality healthcare services than rural communities overall. Since that study, 164 new rural hospitals have closed according to the University of North Carolina’s Shep Center for Health Services Research, further decreasing the already low level of hospital access for rural residents. This data reveals that poor access to health services and low-quality hospital care have been issues in rural communities for many years and have only gotten worse with time.
Many policy experts believe the solution to decreasing healthcare access is mobilizing FSED’s for the purpose of providing emergency care in rural areas. Thus, we must take a closer look at FSEDs and how they function. The American College of Emergency Physicians (ACEP) define an FSED as “a facility that is structurally separate and distinct from a hospital and provides emergency care.” There are two types of FSEDs: Hospital Outpatient Departments (HOPDs) also known as Hospital-Based Off-Campus Emergency Departments (OCEDs) and Independent Freestanding Emergency Centers (IFECs).
HOPDs belong to, and are controlled by, larger medical centers or hospital systems. These systems tend to accept Medicare and Medicaid payments, thereby placing them under the regulatory rules of the Centers for Medicare and Medicaid Services (CMS). The CMS regulations governing HOPD style FSEDs, are the same regulations that most Emergency Departments in the U.S. operate under.
The other style of FSED are IFECs which differ from HOPDs in that they can be owned by individuals or private businesses. CMS does not recognize IFECs as Emergency Departments, which prevents them from taking Medicare or Medicaid payments, and exempts them from the regulations that govern HOPDs and traditional emergency departments. Because of this the regulations for IFECs are incredibly inconsistent and vary by state. Some states have decided to regulate IFECs under guidelines of the Emergency Medical Treatment and labor act (EMTALA), which ensures hospitals treat and stabilize patients regardless of their ability to pay. A handful of states have taken no regulatory action at all, allowing FSEDs to act largely unregulated. Many states will not give licenses for any kind of FSED, and others will only license HOPDs style facilities governed by CMS regulations.
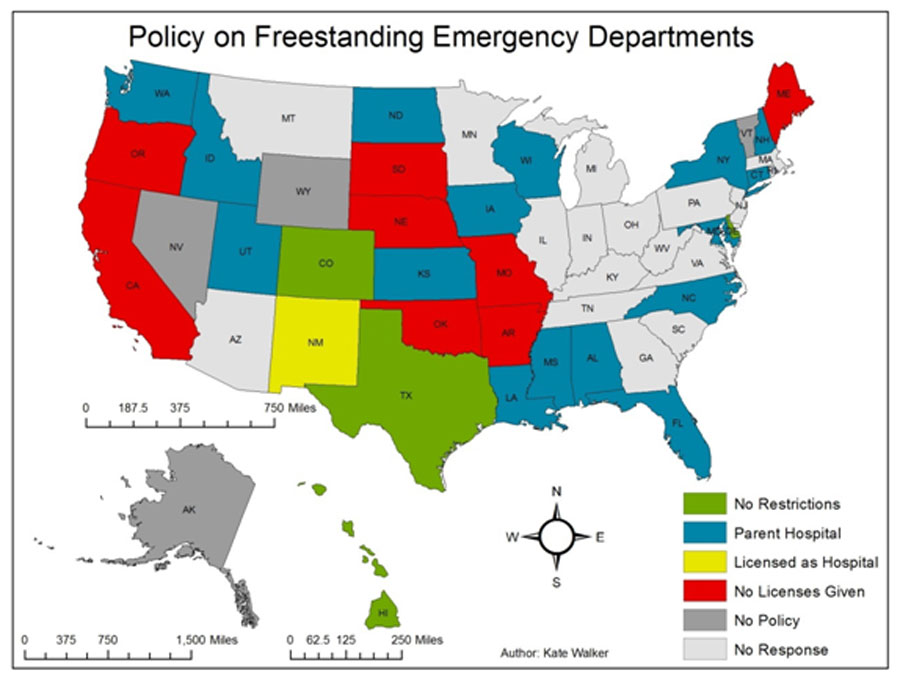
RuralHealthInfo.org | Adapted from “State of the Nation: Policy for Owning and Operating a Freestanding Emergency Department,” (no longer available online) Journal of Free-Standing Emergency Medicine, August 2015
So, who is advocating for this move to Freestanding Emergency Departments as the mode of delivering healthcare in the rural U.S.? In an article from the Rural Health Information Hub discussing FSEDs as an alternative healthcare model for rural communities, the organization spoke to MD and ACEP member David Ernst who advocated for the IFEC model, the model which allows for FSEDs to be privately owned. Ernst argued that independently owned IFECs are more sophisticated, efficient, and economically streamlined compared to other models which are hampered by federal enforcement of Medicare mandates (though Ernst does not explain here what he means by any of these statements specifically.) He also mentions that IFEC facilities tend to thrive in high income urban and suburban areas where most the population has high quality insurance (Lukens, 2016).
How the large-scale implementation of IFEC facilities would improve healthcare quality and access in rural areas is truly a mystery. Anyone who genuinely offers this as a solution likely does not understand the nature or the gravity of the problems facing rural healthcare, and the U.S. healthcare system in general. Most who offer it as a solution likely have contradictory motivations leading them to believe that this is a viable solution.
Let’s take a closer look at what’s causing poor health outcomes for rural Americans. The National Library of Medicine did an analysis of the historical problems in rural healthcare and found that the general lack of rural hospitals is largely due to ‘financing issues,’ as rural healthcare facilities often struggle bringing in enough revenue to remain profitable in sparsely populated rural areas. Additionally, when larger healthcare systems realize they are no longer making a net profit from selling healthcare within a certain geographic area, they have historically chosen to remove healthcare providing facilities from that area, regardless of how it effects the residents in that area. The analysis identified that the primary elements contributing to rural healthcare’s worsening condition are decreasing and disproportionately elderly populations, economic stagnation, high rates of underinsured residents, and the trend towards outpatient over inpatient care (Weisgrau). All the relevant scholarly literature agrees that the most influential problems facing rural healthcare are economic in nature.
These issues highlight the inefficiencies of the market when it comes to protecting the interests of working-class citizens, and the lunacy of the idea that profit driven private companies working within healthcare will prioritize the interests of vulnerable populations over their own monetary interests. In fact, companies could not prioritize population health outcomes even if they wanted to. Market competition rewards those who sell the most healthcare at the greatest margins, but harshly punishes those who would bring healthcare to a population of people who can’t afford to pay both the costs of the healthcare services provided, as well as the profits of the private shareholders who own the facilities providing care.
So now that we have a more concrete understanding of the problems rural healthcare is facing, let’s turn back to the proposed IFEC model to ask whether it truly addresses the economic barriers in rural healthcare? Given that IFECs can’t accept Medicaid payments, it is unlikely that underinsured populations will have access to IFEC care. In many states IFECs can turn away underinsured without giving care, as they are not subject to CMS regulations and therefore EMTALA. For the private business entity who owns the IFEC this is a positive, as IFECs can avoid the revenue loss that traditional hospitals incur from being forced by regulation to provide unpaid care. However, IFECs do nothing to improve deficient access to care for the underinsured, or the 12.3% of rural residents who are completely uninsured (Day, 2019). IFECs may be a less costly way for businesses entities to maintain Emergency Department style facilities in rural areas that can’t support full-service hospitals, but they do little to address the most impactful barriers to healthcare affecting rural citizens. IFECs do nothing to provide healthcare for those who lack insurance coverage, which is one of the foremost barriers to healthcare in the U.S.
The proposed system could easily be exploited by predatory business interests. With a declining number of rural hospitals, business entities could theoretically wait for an area’s hospital to close, then fill the healthcare void in that area by implementing an IFEC style FSED. The facility would be under no obligation to treat those residents who cannot afford to pay for care. They could perform services exclusively for people with income levels high enough to afford them, or those desperate enough to pay more than they can afford. After operating in this manner for a period, the IFEC owners would get an understanding of who in the rural community can afford ED services and how much they’re willing to pay. The facility could then be staffed with only as many employees as necessary for performing those services, decreasing variable costs for the facility, and maintaining sufficient revenue levels for the business owners. Moving towards IFECs would allow healthcare investors to generate revenue in rural areas where they previously could not but would do little to address poor health outcomes for rural populations that need it most.
So why did MD David Ernst promote the IFEC model in his interview with Rural Health Information Hub? Well, it may have something to do with the fact that Ernst is the president of a company that provides telemedicine software to 325 emergency departments and hospitals across the U.S. Ernst thus stands to profit from the implementation of more FSEDs, as the facilities are reliant on telemedicine software to communicate with other facilities. Creating more FSEDs would increase demand for the software produced by Ernst’s EPOWERdoc company. Obviously, there is a conflict of interest here, and Ernst is likely promoting the FSED model to boost his private companies’ revenue. Despite the conflict of interest, Rural Information Hub present Ernst’s interview as if he were an unbiased expert. A clear example of how the solutions to the healthcare systems many problems are being produced by profit driven interests, who do not prioritize the health outcomes of the communities they serve, but rather the revenue of the companies they belong to.
A detailed cost analysis of FSEDs concluded that IFECs would not be financially viable in rural areas, especially if they are not allowed to accept Medicare and Medicaid payments. The analysis also found that the alternative HOPD model has only worked in areas with relatively high population density and favorable payer mixes. They have been far less successful in the sparsely populated and poorer areas of rural America. Hospital systems rarely think it is worth their effort and resources to implement and maintain FSEDs in these areas. Doing so rarely generates revenue and can even work in reverse as a drain on total revenue (Williams, 2015). While FSED implementation may be an improvement in rural areas with no nearby hospitals at all, they are a deeply flawed concept, and one that has been debated since the early 1970s. Bringing high quality healthcare to rural America will require new solutions that seek to enact macro level changes, rather than outdated solutions which have largely failed to address historically prevalent issues.
Conclusion: Socialist Healthcare is the Real Solution
The primary contradiction in rural healthcare, and the healthcare system in its totality, are the profit incentives of the various entities who provide healthcare services and mediate payment. Cuba is a vastly poorer country than the U.S. that has faced an embargo limiting its economic activity for decades. Despite that, Cuba has achieved and maintained universal health care for many years, including the rural and mountainous regions of the island. Since 1959 Cuba has invested substantial resources towards developing their healthcare infrastructure and training new doctors. Cuban doctors receive free medical school in exchange for pledging to serve the rural areas of Cuba for a certain time after graduation. A beautiful example of a policy designed to both train new staff and ensure that the staff serve the neediest parts of the country.
In 1999 Cuba assisted Venezuela in implementing similar policies, as well as an effort to increase the level of preventative care services. Their efforts resulted in a substantial increase in the number of rural clinics, physicians, nurses, and dentists as well as a 30% decrease in ER visits thanks to the newly implemented preventative care (Westhoff). If the U.S. were to implement a similar program, focusing their resources on developing the healthcare system, similar policies to those enacted in Cuba and Venezuela could be implemented on a massive scale. The problem is that Cuba’s reforms required Government initiatives to ensure the nation’s resources were utilized to develop the rural health infrastructure, and train more rural healthcare staff. Government planning was used to do what the free market could not.
The healthcare markets and private hospital systems in the U.S. have shown time and time again that they will not adequately serve rural communities unless it is profitable. In sparsely populated communities across rural America, it is rarely profitable. Thus, the state of rural healthcare can only be improved if the U.S. abandons the dogmatic belief that market forces always generate optimal outcomes for everyone – especially in the realm of healthcare where profit motivations so clearly contradict the effort to create an optimal system for everyone. The healthcare system itself must abandon the idea that it can maintain the current profits that it generates for investors, while also meeting the needs of rural populations. Rational economic planning is what is needed to fix the system’s problems in the future. Rational planning is impossible under the system’s current ownership, whose only rationale is maximizing their own revenue. Workers must seize control of the healthcare system from the shareholders and executives who have captured it and turned it into a profit generating monstrosity. This change in ownership over the healthcare system’s ‘means of production’ is the only way to create a rational system which works to optimize health for the working masses of society.
References
- Lutfiyya, M. N., Bhat, D. K., Gandhi, S. R., Nguyen, C., Weidenbacher-Hoper, V. L., & Lipsky, M. S. (2007). A comparison of quality of care indicators in urban acute care hospitals and rural critical access hospitals in the United States. International Journal for Quality in Health Care, 19(3), 141–149. https://doi.org/
- University of North Carolina. (2022, January 11). Rural Hospital closures. The Cecil G. Sheps Center for Health Services Research. Retrieved April 18, 2022, from https://www.shepscenter.unc.edu/
- Lukens, J. (2016, November 30). Freestanding emergency departments: An alternative model for rural communities. The Rural Monitor. Retrieved April 18, 2022, from https://www.ruralhealthinfo.org/
- American College of Emergency Physicians. (2020, April). Freestanding emergency departments. acep.org. Retrieved April 18, 2022, from https://www.acep.org/
- Weisgrau, S. (1995). Issues in rural health: Access, hospitals, and reform. Health care financing review,17(1),1-14.
- Day, J. C. (2019, April 9). Rates of uninsured fall in rural counties, remain higher than Urban counties. Census.gov. Retrieved April 18, 2022, from https://www.census.gov/
- Williams, J. D., Song, P. H., & Pink, G. H. (2015, November). Estimated costs of rural freestanding emergency departments. ShepsCenter.unc.edu. Retrieved April 19, 2022, from https://www.shepscenter.unc.edu
- Esposito, C. L., Gilbert, J., Ciampa, A., & Markman, J. (2017, August 1). Against All Odds: Cuba Achieves Healthcare for All- An Analysis of Cuban Healthcare. nysna.org. Retrieved April 19, 2022, from https://www.nysna.org
- Westhoff, W. W., Rodriguez, R., Cousins, C., & McDermott, R. J. (2010). Cuban healthcare providers in Venezuela: A case study. Public Health, 124(9), 519–524. https://doi.org
Republished with permission from Midwestern Marx. Photo: “Countryside” by Amy the Nurse on Flickr (CC BY-NC-ND 2.0).